- Have any questions?
- 085913 90567
- drgeorgechestdiseases@gmail.com
Is lung cancer hereditary?

Lung Cancer in Young Adults: Causes, Symptoms, and Hope for the Future
June 12, 2025
Difference between Emphysema and Empyema
July 15, 2025Our lungs play an important role—moving oxygen into our bloodstream and filtering out toxins with every breath. When lung tissue is damaged, our quality of life can deteriorate significantly. Lung cancer, in particular, exacts a heavy toll, both physically and emotionally. Globally, it’s among the leading causes of cancer-related deaths—accounting for an estimated 2.2 million new cases in 2020 alone.
“It’s vital to recognize that your lungs don’t just reflect your breathing habits—they also carry your family’s genetic legacy,” explains Dr. George, a distinguished Thoracic Surgeon in Mumbai. “While smoking remains the most significant risk factor for lung cancer, inherited genetics also play an important role. Awareness can guide early screening and proactive prevention.”
This blog dives deeper into what heredity means for lung cancer—why it matters, how genetics come into play, and what you can do if it runs in your family.
Why This Question Matters Today
Lung cancer is often associated with smoking, but not everyone who develops it has ever smoked. In fact, around 10–20 % of lung cancer cases globally occur in individuals who have never lit a cigarette. In India, lung cancer is responsible for approximately 63,000 cancer-related deaths in men and 17,000 in women annually. A 2022 cancer registry revealed that cases among non-smokers are increasing—now constituting nearly one-fifth of all lung cancers detected. This context makes genetic predisposition a key part of the discussion.
Genetic advances have brought clarity to many hereditary issues. Identifying one’s susceptibility not only opens up possibilities for early detection but also provides peace of mind and a framework for personalized prevention strategies.
Worried about a family history of lung cancer? Consult a medical professional to explore personalized risk assessment and preventive strategies today.
Family History and Lung Cancer Risk
Unlike single-gene diseases such as Huntington’s or cystic fibrosis, hereditary lung cancer is often the result of multiple genetic risk factors combined with environmental exposure. However, research indicates that individuals with a close relative—especially a first-degree relative like a parent or sibling—who had lung cancer are at a 1.5 to 2 times higher risk of developing the disease themselves than the general population.
Dr. George, a prominent lung cancer specialist in Mumbai, clarifies the science behind it,
“Inherited mutations in genes can tip the scales—but they aren’t definitive predictors. Purely hereditary forms of lung cancer are relatively rare. Most often, family history reflects a combination of shared genetics and shared environments—such as exposure to indoor air pollution, radon, or passive smoke—which can cause inaccuracy in the risk assessment.”
Want to learn about hereditary lung cancer syndromes? Let’s unpack that next.
Lung Cancer Without Smoking: The Hereditary Angle
While smoking is the top culprit, not every case of lung cancer circles back to tobacco. Hereditary lung cancer syndromes can play a significant role, especially in individuals who have never smoked. Key syndromes associated with hereditary lung cancer include:

EGFR Mutation-Positive Lung Cancer:
These mutations appear more frequently in never-smokers and may be inherited across generations
Targeted therapies offer effective treatments for patients with this mutation
Li-Fraumeni Syndrome (TP53 gene)
Caused by inherited mutations in the TP53 tumor-suppressor gene
Increases the risk of lung cancer along with a variety of other cancers, often at a younger age
HER2 and KRAS Genetic Variants
Less common but still notable in cases of familial lung cancer where other typical risk factors are absent
Other Rare Syndromes
Certain inherited rarer syndromes—such as those involving DNA repair defects—may have a small but important correlation with lung cancer risk
Dr. George, an experienced oncologist in Mumbai, adds,
“Hereditary lung cancer syndromes may be uncommon, but they carry high stakes. If multiple relatives—especially non-smokers—develop lung cancer at younger ages, getting tested for syndromes like Li Fraumeni or EGFR mutations can provide clarity and open doors to early treatment options.”
Unsure whether your family history signals hereditary risk? Speak with a pulmonologist or genetic counselor to determine if genetic testing is right for you.
Next, we discover the role of genetic testing!
Should You Get Genetic Testing for Lung Cancer Risk?
Deciding whether to pursue genetic testing involves a thoughtful evaluation of several factors:
Family history: Multiple affected relatives, the presence of lung cancer in younger generations, or clustering of different cancers may tip the scales toward testing.
Age of diagnosis: Lung cancer before age 50 may indicate genetic predisposition.
Non-smoker status with lung cancer: Testing is more strongly recommended when lung cancer develops in someone who has never smoked.
A typical testing pathway might involve panels that screen for EGFR, TP53, and other genes linked to lung cancer risk. Testing helps in designing surveillance programs—like earlier or more frequent low-dose CT scans—and may guide preventive strategies or enrollment in clinical trials.
Dr. George, a leading lung-health expert practicing in Mumbai, shares his insight,
“There are limitations: not all genetic variants are fully understood, and uncertainty may remain even after testing. Genetic counseling is essential both before and after the test to discuss implications, family impact, and next steps. When used responsibly, along with family history and clinical evaluation, they provide the best insight for tailored monitoring and prevention.”
Keep reading—up and discover how to best manage your risk.
Prevention & Monitoring if You Have a Family History

While you can’t change your genes, there are proactive steps you can take:
Quit Smoking: Even in families with minimal smoking history, tobacco compounds inherited risk.
Address Environmental Hazards: Test your home for radon, keep indoor air clean, and avoid heavy pollution where possible.
Follow Personalized Screening Plans: Those with strong family histories may begin annual low-dose CT scans earlier than the average screening onset.
Adopt a Healthy Lifestyle: A balanced diet, regular exercise, and maintaining healthy weight contribute to overall resilience—even if they don’t remove genetic risk entirely.
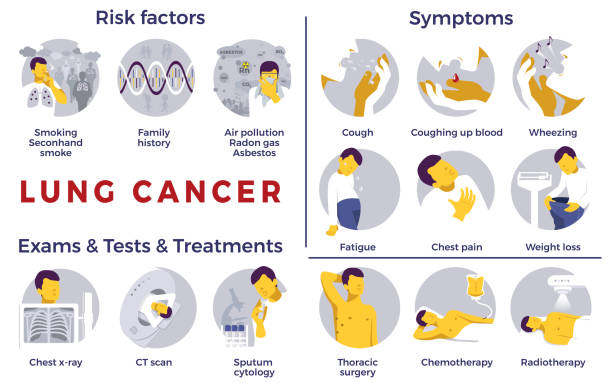
Stay Vigilant with Symptom Awareness: Early signs such as persistent cough, unexplained breathlessness, chest pain, or sudden weight loss should prompt immediate evaluation—especially with hereditary context.
Seek Expert Guidance: Regular visits with pulmonologists, oncologists, and genetic counselors allow for timely decision making and possible participation in preventive programs or clinical trials.
Final Thoughts: Genetics Are a Piece of the Puzzle
Hereditary lung cancer doesn’t follow a simple “one gene, one disease” pattern. It results from an interplay of genetic variants, environmental factors, and lifestyle habits. Family history can raise valid concerns—but it is not a sentence.
Genetic testing, when used wisely, empowers you with knowledge—not fear. With regular screening, concerted preventive measures, and expert counsel, individuals with a family history or known genetic risk can still live long, fulfilling lives.
Concerned about a genetic predisposition to lung cancer? Connect with a healthcare professional for personalized risk evaluation and a tailor-made surveillance plan.
Before you go—get clear answers to your top FAQ.
FAQ
Question 1. Can I inherit lung cancer even if I’ve never smoked?
Answer: Yes. While genetic risk is less common than environmental causes, inherited mutations—like EGFR or TP53—can lead to lung cancer in those who have never smoked. Having a family member diagnosed at a younger age, particularly among non-smokers, can suggest a hereditary factor.
Question 2. Is genetic testing covered by insurance?
Answer: Coverage varies. In India, public insurance schemes and private providers may approximate certain genetic tests, especially for high-risk individuals with documented family history. Always check policy fine print and consult your provider directly.
Question 3. What are the early signs I should watch for?
Answer: Be alert to symptoms such as:
· Persistent cough lasting more than a few weeks
· Sudden breathlessness or wheezing
· Unexplained chest pain
· Recurrent lung infections
· Unintentional weight loss, fatigue
Question 4. How common is inherited lung cancer?
Answer: Purely hereditary lung cancers are relatively rare—perhaps under 5 % of all cases. But roughly 15–20 % of lung cancers occur in non-smokers, and a subset of those may involve genetic predisposition.
Question 5. Can lifestyle changes still help if I’m genetically at risk?
Answer: Absolutely! Avoiding tobacco, reducing exposure to environmental pollutants, adopting a balanced diet, exercising, and following preventative screenings all significantly lower your risk—even if you carry genetic markers.
Ready to take charge of your lung health and genetic risk? Speak with a medical expert today to craft a proactive plan tailored to your family history and lifestyle.
References:
https://my.clevelandclinic.org/health/diseases/4375-lung-cancer
https://www.webmd.com/lung-cancer/is-lung-cancer-genetic
Disclaimer: The information shared in this content is for educational purposes only and not for promotional use.