- Have any questions?
- 085913 90567
- drgeorgechestdiseases@gmail.com
Can You Get Lung Cancer Without Smoking?

Empyema vs Pleural Effusion: What’s the Difference?
February 13, 2025
Lung Cancer from Air Pollution
March 12, 2025Can You Get Lung Cancer Without Smoking?
Lung cancer is one of the most commonly diagnosed cancers worldwide, with over 2.2 million new cases each year. In India, it makes up about 5.9% of all cancer cases, and an increasing number of non-smokers are being diagnosed. Although smoking is the primary cause, non-smokers can also develop lung cancer due to environmental and genetic factors, highlighting the importance of early detection since the disease often shows no symptoms until advanced stages.
“Many non-smokers are shocked when they receive a lung cancer diagnosis because they never considered themselves at risk,” says Dr. George Karimundackal, a leading thoracic surgeon and lung cancer specialist in Mumbai, India. “The key to combating lung cancer in non-smokers is awareness, early screenings, and proactive lifestyle changes.”
With decades of experience, Dr. Karimundackal has helped countless patients navigate lung cancer treatment through advanced screenings and personalized approaches, significantly improving patient outcomes and survival rates.
Think only smokers get lung cancer? Let’s delve into why non-smokers are also at risk.
Lung Cancer: It’s Not Just a Smoker’s Disease

Lung cancer is often considered a “smoker’s disease,” causing many to believe that only smokers are at risk. However, studies show that 10-20% of lung cancer cases occur in non-smokers, who are increasingly recognized as a significant portion of lung cancer statistics. While smoking is the leading risk factor, environmental pollutants, secondhand smoke, and genetics can also contribute to the disease.
This misconception can lead to delayed diagnosis and treatment for non-smokers, as they often do not see themselves as at risk, causing symptoms to go unnoticed until the disease is advanced. Raising awareness and promoting early screenings are crucial for improving survival rates. Acknowledging that lung cancer affects non-smokers is essential for better prevention and treatment.
What causes lung cancer if not smoking? Let’s explore the hidden risks that many overlook.
Causes of Lung Cancer in Non-Smokers
While smoking is the primary cause of lung cancer, non-smokers should also be mindful of their lung health. Here are key risk factors to consider:
1. Radon:
Radon is a naturally occurring radioactive gas found in soil and rock. It can build up in homes, especially in basements and areas with poor ventilation. Prolonged exposure to high levels of radon is one of the leading causes of lung cancer in non-smokers.
2. Polluted Air

Air pollution, especially fine particulate matter (PM2.5), is a significant contributor to lung cancer. Pollutants from vehicle emissions, industrial waste, and even indoor cooking fumes can damage lung cells over time.
3. Secondhand Smoke

Even if you don’t smoke, prolonged exposure to secondhand smoke can increase your lung cancer risk. Passive smoking exposes non-smokers to harmful carcinogens, making them vulnerable to the same risks as active smokers.
4. Occupational Hazards
Certain occupational hazards can expose non-smokers to carcinogenic substances, increasing lung cancer risk. Industries involving asbestos, arsenic, diesel exhaust, and silica dust pose significant dangers.
5. Diet
A diet lacking essential antioxidants and vitamins can weaken the body’s defences against cancer. Studies suggest that diets rich in fruits and vegetables can help protect against lung cancer by reducing oxidative stress and lung inflammation.
Did you know lung cancer comes in different types? Let’s dive into the most common ones found in non-smokers.
Understanding the Different Types of Lung Cancer in Non-Smokers
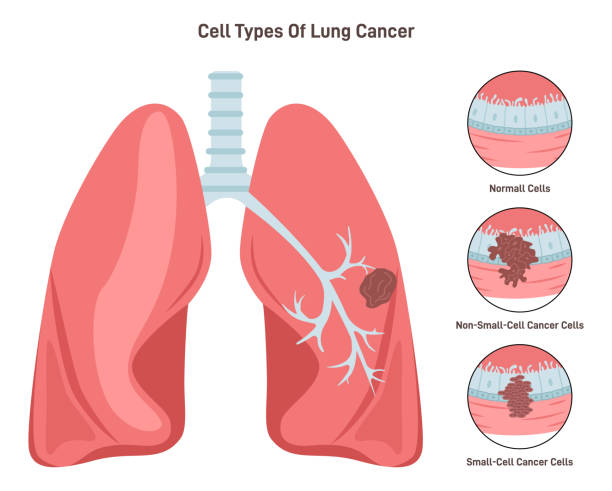
1. Adenocarcinoma
Adenocarcinoma is the most common lung cancer in non-smokers, especially among women. It forms in the outer parts of the lungs and tends to grow slowly, making early detection difficult. This type is often linked to genetic mutations rather than external carcinogens.
2. Large Cell Carcinoma
This is an aggressive and fast-growing form of lung cancer that can appear in any part of the lung. It is less common in non-smokers but can be more challenging to treat due to its rapid spread.
3. Small Cell Lung Cancer (SCLC)
Although rare in non-smokers, small cell lung cancer (SCLC) is an aggressive type that spreads quickly. It is typically associated with heavy smokers. However, in some cases, genetic factors may contribute to its development in non-smokers.
4. Carcinoid Tumors
Carcinoid tumors are a rare and slow-growing form of lung cancer. Unlike other types, these tumors originate from neuroendocrine cells, which help regulate hormones. They usually grow in the central airways of the lungs and may not spread as aggressively as other lung cancers.
5. Lung Nodules & Pre-Cancerous Growths
Some non-smokers develop benign or pre-cancerous lung nodules, which may or may not turn into lung cancer. Regular screenings and follow-ups are essential to monitor their growth and detect cancer in its early stages.
Are there warning signs of lung cancer in non-smokers? Let’s break down the symptoms to watch out for.
Symptoms of Lung Cancer in Non-Smokers

Lung cancer in non-smokers often develops silently, with symptoms appearing only in later stages. Since many non-smokers don’t consider themselves at risk, early warning signs may be ignored. Below are a few signs of lung cancer in non-smokers to watch for:
Common Symptoms:
✅ Persistent cough – A long-lasting cough that doesn’t go away or worsens over time.
✅ Shortness of breath – Difficulty breathing, even during light activities.
✅ Unexplained weight loss – Losing weight without changes in diet or exercise.
✅ Fatigue and weakness – Constant tiredness that doesn’t improve with rest.
✅ Chest pain – Discomfort or pain in the chest that worsens with deep breaths or coughing.
✅ Frequent lung infections – Recurring pneumonia or bronchitis without a clear cause.
✅ Hoarseness or voice changes – A persistent change in voice, often deeper or raspier.
✅ Coughing up blood – Even small traces of blood in mucus can be a warning sign.
✅ Wheezing or noisy breathing – A whistling sound while breathing due to airway obstruction.
✅ Swelling in the face or neck – Caused by a tumor pressing on blood vessels.
Less Common Symptoms:
Bone pain – Pain in the back, ribs, or hips, indicating cancer spread.
Headaches and dizziness – Can occur if lung cancer spreads to the brain.
Difficulty swallowing – Tumor growth may obstruct the oesophagus.
Early symptoms can be subtle but life-saving if caught in time. Consult an experienced specialist for a lung health check-up. Book an appointment now!
Want to lower your chances of developing lung cancer? Let’s discuss practical ways to protect yourself.
How to Reduce Your Risk

While some risk factors, like genetics, cannot be changed, many environmental and lifestyle factors can be controlled. By making informed choices and adopting healthier habits, we can lower the risk of lung cancer in non-smokers. Here’s how:
1. Test for Radon at Home: Get your home tested for radon levels and ensure proper ventilation in basements and lower floors.
2. Reduce Exposure to Air Pollution: Use air purifiers, limit outdoor activities on high-pollution days, and wear masks in highly polluted areas.
3. Avoid Secondhand Smoke: Avoid smoke-filled environments, advocate for smoke-free spaces, and encourage loved ones to quit smoking.
4. Maintain Workplace Safety: Follow safety measures, wear protective gear, and ensure proper ventilation in hazardous environments.
5. Eat a Lung-Healthy Diet: A diet rich in antioxidants, vitamins, and healthy fats supports lung health. Include fruits, vegetables, nuts, whole grains, and omega-3 fatty acids while avoiding processed foods and excessive alcohol.

6. Exercise Regularly: Physical activity strengthens lung function and reduces cancer risk. Aim for at least 30 minutes of moderate exercise most days of the week.
7. Avoid Exposure to Harmful Chemicals: Household and workplace chemicals may contain carcinogenic substances. Use natural, non-toxic cleaning products and avoid prolonged exposure to paints, solvents, and pesticides.
8. Stay Hydrated: Water helps flush toxins from the body and maintains healthy lung function. Drink plenty of water daily to keep your lungs clear of mucus buildup and pollutants.
9. Manage Stress and Get Enough Sleep: Chronic stress and poor sleep can weaken the immune system. Practice stress-reducing activities like meditation and Yoga and ensure 7-9 hours of sleep each night.
10. Schedule Regular Health Check-Ups: Early detection significantly improves lung cancer non-smoker survival rates. Get regular lung screenings if you have risk factors such as a family history of lung cancer or frequent exposure to pollutants.
Taking Charge of Your Lung Health: A Message of Hope
A lung cancer diagnosis can be overwhelming, especially for non-smokers who didn’t expect to be at risk. Fortunately, advances in early detection, targeted therapies, and lifestyle changes are improving survival rates.
You can enhance lung health by minimizing environmental risks, maintaining a healthy lifestyle, and scheduling regular check-ups with seasoned professionals like Dr. George Karimundackal. Staying informed and making small changes, like improving indoor air quality and avoiding secondhand smoke, can contribute to a healthier future.
Your lung health is in your hands. If you have concerns or want expert guidance, reach out to a specialist and take charge of your well-being today.
Frequently Asked Questions:
1. What is the most common lung cancer in non-smokers?
Adenocarcinoma is the most common lung cancer in non-smokers. It forms in the outer regions of the lungs and tends to grow more slowly than other lung cancers. Unlike smoking-related lung cancers, adenocarcinoma in non-smokers is often linked to genetic mutations like EGFR, ALK, and ROS1, making targeted therapy a viable treatment option.
2. What factors increase the lung cancer risk for non-smokers?
Several factors contribute to the risk of lung cancer in non-smokers, including exposure to radon gas, air pollution, secondhand smoke, occupational carcinogens (like asbestos and diesel exhaust), poor diet, genetic predisposition, and chronic lung infections. Even frequent exposure to cooking fumes, especially in poorly ventilated spaces, has been linked to increased lung cancer risk.
3. Is lung cancer in non-smoking females different from that in smokers?
Lung cancer in non-smoking females differs biologically and genetically from lung cancer in smokers. Non-smoking women are more likely to develop adenocarcinoma, and studies suggest hormonal influences and genetic mutations (such as EGFR and ALK mutations) play a significant role. In contrast, lung cancer in smokers often involves squamous cell carcinoma or small cell lung cancer, which have different treatment responses.
4. Can secondhand smoke cause lung cancer in non-smokers?
Prolonged exposure to secondhand smoke significantly increases the risk of lung cancer in non-smokers. Secondhand smoke contains over 7,000 toxic chemicals, many of which are known carcinogens that can damage lung tissue over time.
5. What are the early signs of lung cancer in non-smokers?
Early signs of lung cancer in non-smokers can be subtle and include persistent coughing, unexplained shortness of breath, chest discomfort, fatigue, unexplained weight loss, and frequent respiratory infections. Since non-smokers don’t typically consider themselves at risk, these symptoms are often overlooked until later stages.
6. What is the survival rate of lung cancer in non-smokers?
The lung cancer non-smoker survival rate depends on the stage at diagnosis. Early-stage lung cancer has a much higher survival rate, with localized adenocarcinoma having a 5-year survival rate of around 60-70%. However, late-stage diagnoses have lower survival rates, emphasizing the importance of early detection.
7. Can lung cancer in non-smokers be cured?
If detected early, lung cancer in non-smokers can be effectively treated or even cured with surgery, targeted therapy, and advanced treatments. The lung cancer non-smoker survival rate is higher when diagnosed at an early stage.
Reference links:
http://www.yalemedicine.org/conditions/lung-cancer-in-nonsmokers
https://www.webmd.com/lung-cancer/non-smoker-lung-cancer
Disclaimer: This page is for informational purposes and not for promotional use.